“Do me a favour, speed it up, speed it up.” That is what Donald Trump has been saying to the executives of pharmaceutical companies about their quest for a vaccine for the coronavirus. He has been told very clearly, not least by Anthony Fauci, director of the US National Institute of Allergy and Infectious Diseases (NIAID), that a vaccine will take at least a year to 18 months to develop. But, wrote H Holden Thorp, editor-in-chief of Science in mid-March in an uncharacteristically furious outburst at the US president, “Apparently, Trump thought that simply repeating his request would change the outcome.”
The remark was, you might say, classic Don: petulant, heedless of inconvenient truths and spectacularly ignorant. (He reportedly crowned it with a botched offer of “large sums of money” to a German manufacturer to produce a putative vaccine exclusively for use in the United States.) But one can sense some of that same impatience in the air more broadly: why is there going to be no pharmaceutical magic bullet to get us through this crisis, but only one that will mop up afterwards?
Here, though, is the harsh truth: there will almost certainly be no vaccine ready to use against the Covid-19 virus until early 2021, and perhaps not before the summer of that year.
A typical timescale for developing a vaccine is 15-20 years—remember that there is still no vaccine against HIV today. The only way a coronavirus vaccine could be created as fast as this is by taking new approaches and judiciously cutting corners—for example, by taking some steps of the process that would normally be done sequentially and doing them simultaneously. “This is actually going very fast,” says virologist Barney Graham, deputy director of the Vaccine Research Center at the NIAID.
Already there are candidate vaccines entering clinical trials, the first stage of which is to test for safety in humans. This is remarkable for a new virus that was only recognised in late December. These trials are one thing you just can’t rush—it takes time to be reasonably sure there are no nasty side-effects, irrespective of the enormity of the crisis or of orders barked by Trump or anyone else. As this is a treatment that might ultimately be given to a significant proportion of the world’s population, fast-tracking these checks could be catastrophically dangerous.
Assessing the potential toxicity and side-effects is only one bottleneck, however. Among other issues, there’s the matter of how to mass-produce and distribute a vaccine. Still, researchers are hopeful that we’ll get there—so that there will be a defence against a possible seasonal recurrence of the virus. Big Pharma gets a bad press, but if by the middle of next year we all have immunological protection against Covid-19, it will be an extraordinary testament to the power of modern science to deliver.

Vaccines work by stimulating our immune system into producing defences against the virus. The trick is to confront the immune system with some foreign agent that can mimic the pathogenic virus closely enough without inducing the same nasty symptoms. Edward Jenner discovered the first vaccine in the late 18th century. As a country doctor, he had noticed that milk maids who caught cowpox (which produced pox spots but was otherwise harmless) seemed immune to deadly smallpox. So, in an experiment that would never pass ethical guidelines today, he administered fluid from a cowpox blister to a young boy, and later exposed him to smallpox; the boy’s continued health showed that cowpox indeed conferred immunity. Most vaccines in modern times have used an inactivated or weakened form of the real virus to kick the immune response into action. But today there are new approaches that don’t rely on viruses at all—and if a coronavirus vaccine appears any time soon, it will most probably derive from one of these.
The Covid-19 virus has the unwieldy official title Sars-CoV-2: the medical syndrome Covid-19 is to the Sars-CoV-2 virus as Aids is to HIV (the “19” simply denotes 2019, the year of discovery). It is just one of a family of coronaviruses, including the one that caused the 2002 Sars (severe acute respiratory syndrome) epidemic in which about 800 people died. Similarly, a coronavirus was responsible for the Mers (Middle East respiratory syndrome) in 2012. Other coronaviruses can cause varieties of the common cold. Like the highly virulent forms of flu, such as bird flu (a viral strain called H5N1) and swine flu (H1N1), they come from animals, having mutated into a form that can attack humans. In the case of this emerging pandemic, like the Sars virus before it, the coronavirus seems to have originated in bats in China.
Viruses are the ultimate Darwinian machines. They lie on the borderline of what scientists consider to be alive: not true organisms, since they have no means of replicating on their own or obtaining energy by metabolism. They can proliferate only by piggy-backing on the resources of the hosts they infect. They are little more than genetic material—many not even containing DNA, but rather, the closely related chemical compound called RNA—packaged in a protective shell: “bad news wrapped up in a protein,” as the biologist Peter Medawar put it. The shell of coronaviruses, like that of some other common pathogens such as flu, HIV and Ebola, is in fact made of fatty lipid molecules, similar to those that make up our own cell membranes, but is studded with proteins that become attached to the cells the virus invades. This lipid coat can be dissolved or disrupted by soap or alcohol, which is why handwashing and sanitisers confer some protection.
The sole aim of viruses is to invade the cells of the host organism and commandeer its molecular machinery to produce more copies of itself. Sometimes—as, for most people, with flu—this temporary invasion leaves us depleted and suffering from the inflammatory response of the immune system doing its best to fight off the invader: a runny nose due to overproduction of protective mucus, and fever as the immune response goes into overdrive. But for people who are already weakened by age or illness, the consequences of these defensive reactions are fatally debilitating.
“There are new approaches that don’t rely on viruses at all”
If the virus is more virulent, as with Sars or Ebola, the resulting complications from, say, respiratory failure or tissue rupture create a much higher fatality rate: around 10 per cent of those who got Sars died, and 30 per cent for Mers. Like those pathogens, the Covid-19 coronavirus attaches to cells in the airways and lungs, wreaking havoc. If the immune system kicks in fast and strong, it can clear the infection without serious symptoms. But if it can’t—or if the response is delayed, and it then tries to over-compensate to clear the higher levels of virus—the consequences can be serious, even fatal: the lungs may become filled with fluid, potentially leading to acute respiratory failure and the need for urgent and intensive medical intervention.
The Covid-19 coronavirus has just the kind of properties to make a pandemic both hard to avoid and catastrophic. It is highly contagious: typically a person who catches it will infect around 2.5 others, while that number is just 1.3 for seasonal flu. (Any number above 1 will eventually produce exponential growth of infection unless checked.) The fatality rate, which seems to be around 1-2 per cent, is high enough to create massive mortality amid a pandemic, while not so high that it retards the virus’s progress by killing too many hosts too quickly. And unlike Sars, where infected individuals fell ill very quickly, the coronavirus can become infectious probably for a day or two before a person experiences any symptoms, allowing them to go about their ordinary business and pass the virus on unawares.
When the first cases of Covid-19 were recognised in a hospital in Wuhan at the end of December, they were thought to be a form of Sars. But the Chinese scientists who isolated the virus responsible and sequenced its genome discovered that it was a new, albeit related, type. They released their findings on 10th January, although already, over in the US, Graham says “we’d heard a rumour a few days earlier that it was going to be a coronavirus, so we were preparing to act” based on their knowledge of Sars and Mers.
The first step is to understand what you’re dealing with, and the genome is the place to start. Viral genomes tend to be very compact and economical: they mostly encode the few proteins it needs to do its dirty work. It is these proteins that our immune system must learn to recognise in order to develop immunity.
When the immune system is challenged by some agent from outside the body, it generates a massive, random library of molecules called antibodies in the hope of producing one with the right shape and chemical properties to latch onto the invading particles and prevent them from infecting cells. At the same time, the immune system quickly learns to recognise cells that have become infected, whereupon those cells are destroyed by specialised “killer T cells,” so that they will not produce more virus. A vaccine trains the immune system to make the right antibodies against the invading pathogen. Once it has learnt, it remembers: you’ve got immunity. (One key unknown for the coronavirus is how long this memory lasts—it may be that, as with flu, annual vaccination will be needed to prevent seasonal outbreaks.)
Vaccines that rely on a weakened form of the virus to raise the alarm are complicated to make—you have to be able to disarm it enough to be safe, but still to generate the right response. And making large amounts of an entirely engineered virus is hard.

There are alternatives. Sometimes it can be enough merely to present the body with one of the viral proteins: innocuous on its own, but adequate to trigger the immune system into producing the right defences. Purely protein-based vaccines do exist, for example against hepatitis B. But they, too, have their drawbacks. Proteins are complicated molecules, and pretty much the only way we have of making them at large scale is by genetic engineering: inserting the viral gene encoding the relevant protein into another kind of cell (typically from a mammal, insect or yeast) so that it will churn out the protein. That’s a challenging and expensive way to make the vaccine at large scale.
___________________________
Read more: Paul Young explains what it's like
to be working on a vaccine
___________________________
Many companies seeking a coronavirus vaccine are taking another, even newer option, in which our own cells are persuaded to make the immune-triggering viral protein themselves. All proteins, whether human or viral, are encoded in a gene (in DNA for human, DNA or RNA for viruses); converting that information to the protein involves an intermediate stage in which the genetic information is first used to build a molecule called messenger RNA (mRNA). Cells have a piece of molecular machinery called the ribosome that translates this mRNA message into the relevant protein molecule; viruses hijack this to make their own proteins and thus to replicate. So-called “mRNA vaccines” contain strands of the mRNA molecule that encode the viral protein selected to elicit production of antibodies; for the coronavirus this will be one of the “spike” proteins that sticks out from the virus’s shell and helps it gain access to our cells. Deliver the right piece of mRNA to the body, and it makes the protein that activates the desired immune response. “Your own muscle cells are the protein factory,” says Graham, who is pursuing this approach at NIAID.
He and his colleagues knew it could work, because they had already tried it for the Mers coronavirus, to promising effect. “We know this vaccine approach is very potent in small animals, and we think it will be in humans,” he says.
The big advantage is speed: mRNA can be synthesised by chemical methods, not complicated microbiological fermentation. “We’ve done a lot of different types of vaccine in the past, but mRNA, because of its manufacturing platform, is faster,” says Graham. “Our goal here is to use something that would be ready for a larger-scale trial by the winter [of 2020-1], and we thought that this would be our only chance to achieve that.”
There’s a further advantage. Because the viral protein is actually being made inside our cells, it not only stimulates production of the virus-blocking antibodies but also activates the immune system to produce the killer T cells that can identify and clear infected cells from the body. That means infected people given the vaccine should have a reduced period of infection.
There’s just one hitch: no mRNA vaccine has ever been licensed for human use before. The potential advantages and the severity of this crisis, however, are enough to persuade drug companies that it’s worth the gamble.
The first candidate mRNA vaccines for this new coronavirus were announced in late February—remarkably, a mere matter of weeks after the identity of the virus was pinned down and published in January—by Moderna, a biotech company in Cambridge, Massachusetts. The first human tests, initially for safety on non-infected volunteers, began—with unprecedented speed—in Washington state in mid-March, under the auspices of the NIAID. Graham has said that mice tested with the vaccine have already shown a similarly positive protective response to the one elicited by a candidate mRNA vaccine against Mers.
The safety trials are crucial—and stringent. “Vaccines have a very high safety bar,” explains Graham, “because they are given to healthy people”—if you’re administering it to huge numbers of well people, you need to be sure that the drug itself doesn’t cause any illness. The territory is not, however, completely unchartered. For example, the German company CureVac—the object of Trump’s “US-only” overtures—began trialling an mRNA vaccine for rabies in humans in 2015, and it plans to start clinical trials with its own coronavirus vaccine in the summer. (Clinical trials are also planned for mRNA vaccines against flu and herpes.) “Hopefully by this summer we will be in a position to say it is safe and reasonable to put this into a larger number of people —say, 500 or so,” says Graham.
There are many other vaccine candidates in development. For example, Inovio Pharmaceuticals in Pennsylvania, collaborating with a Chinese biotech company, also has human clinical trials due to begin in April. Giants such as GlaxoSmithKline and Johnson & Johnson are in the race too: the former is collaborating with Chinese-based Clover Biopharmaceuticals on a protein-based vaccine.
Normally, the “Phase I” safety trials are followed by Phase II trials to look for efficacy—how effective is the drug in treating the target disease—and then the final Phase III trials involving large-scale human testing on perhaps several thousand patients. But there are hopes that regulators will be prepared to fast-track these, and already the research is moving forward in an unusual way. Tests to see how effective the vaccines are in animals, for example, are happening in parallel to, rather than in advance of, the human safety tests.
Mark Feinberg, president and CEO of the International Aids Vaccine Initiative, who worked on Ebola vaccines, has justified this novel shortcut, telling the online medical news service StatNews that “I personally think that’s not only appropriate; I think that’s the only option we have.”
Vaccines aren’t the only way to combat a viral pandemic like Covid-19. It might also be possible to develop antiviral drugs that block or mitigate the effects in infected people, typically by disrupting viral replication. For flu, such drugs offer only imperfect protection, tending only to be effective if taken early enough after infection. But antivirals are all we have to fight HIV—and yet they have proved to be enough to stop it being the death sentence it used to be, by preventing the development of Aids symptoms in infected people.
Some of the same antivirals developed to combat HIV are now being experimentally tested in China on coronavirus patients, too, with—according to tentative and very early reports—some encouraging results. But many experts think that such drugs will need to be tailored specifically to coronaviruses to do a good enough job.
Another currently being trialled is called remdesivir, and was originally developed by California-based Gilead Sciences to treat Ebola. It didn’t work well enough with that singularly deadly disease, but it has shown some effect against Sars and Mers. Since its safety has already been tested, Gilead is said to be already conducting Phase III trials on several hundred people with Covid-19 in Wuhan. However, one small test conducted already on just three people in the US hospitalised with the virus has been reported to have had rather disappointing results—the efficacy was unclear, and there were some troubling side-effects.
In any event, vaccines are the only way to prevent people from actually catching Covid-19. Without them, the virus will remain in the human population at a low level even when the peak of the pandemic has passed, so that another outbreak will always be possible. So a vaccine that is both safe and effective is essential for the long term.
For all its urgency, though, securing this is only the first stage of the battle. We’ll also have to make and distribute vast amounts of the stuff—and figure out who pays for it. “There’s a lot of different bottlenecks along the way in the supply chain for making seven billion doses of a vaccine,” says Graham. CureVac says it is confident that, if its vaccine is approved, it could scale up manufacture to billions of doses. But epidemiologist Roy Anderson of Imperial College London believes there are only five companies in the world with the capacity to manufacture it on the scale that will be needed globally.
“This is also a problem the world needs to manage better,” says Graham: we can’t afford to have all our eggs in so few baskets, not least because it potentially slows the speed of response. “We need to have more distributed manufacturing capacity around the world, so that regions can handle their diseases before they spread,” he says. “That’s something that would be in all of our best interests.”
And we need to solve these issues urgently. After Sars, Mers and bird flu, no one doubts that we will see more lethal epidemics and pandemics. Chinese virologist Shi Zhengli, who worked on the Sars-CoV-2 genome sequencing, has identified bats as a natural reservoir of many Sars-like viruses and says that what we’ve seen so far may be just the tip of the iceberg: there may be as many as 5,000 more coronavirus strains in bats worldwide. New pathogenic viruses tend to transfer to humans in places where populations have encroached on wild-animal habitats—a process that, Graham says, is only going to continue as the human populations grows and the wilderness is driven back.
“Covid-19 has made it painfully apparent how ill-equipped we are”
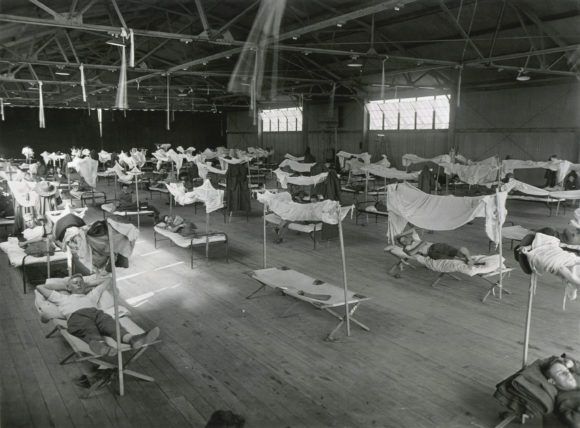
Covid-19 has made it painfully apparent how ill-equipped we are to contain these diseases, and just how vulnerable the economy is to them. While Covid-19 fatalities are concentrated among elderly people, we cannot assume that the same thing will be true with the next pandemic. The 1918 Spanish flu was equally lethal to young, healthy adults and to children. The desperation to find a vaccine might be even more anguished if children were more vulnerable to a future pandemic.
While it might not seem like it (especially to Trump), the coronavirus experience is, in fact, demonstrating that science is far better equipped than it was even a decade ago to respond effectively: to identify and characterise the virus very fast, and to know how and where to start the hunt for a vaccine. Graham points out the extraordinary contrast with Aids, little more than a generation ago. It took two or three years to even discover the HIV pathogen: “It’s remarkable to me that now you have a new virus, you discover it and sequence it and within days you have a test kit,” he says. “This is amazing. People need to understand that technology has made that possible.”
But there are aspects of the vaccine process that can’t safely be rushed, and also still alarming holes in our knowledge. Indeed, we might do well to count our blessings. We were lucky, says Graham, that this was a coronavirus. “We happen to have been working on this a lot and so we felt like we knew what to do immediately. But that’s not true for all the other virus families.” If this had been an arenavirus, for example—a class of rodent viruses that can sometimes jump to humans, for example as the cause of Lassa fever—Graham says that “we would have had to spend months or years deciding how to design a vaccine.”
“We need to generate data on prototypic pathogens in each of these families so that we would know better what to do for the next emerging infection,” he says. While there are over a hundred viral families known on earth, only a few dozen of them cause disease in humans. “So it’s a finite problem that we could manage better and more proactively,” says Graham.
We also need to recognise the pandemic not as a national crisis: something to be sorted by “US-only” or “anywhere-only” arrangements. Nor is it something for which we can or should attribute blame (despite some shameful calls for “reparations” from China) or expect immediate technological fixes. It is a crisis for humanity the planet over, arising from the way we lead our lives today. “We need to look at it as a global problem and not just a national or local one,” says Graham. “A problem anywhere is a problem everywhere.”












