THE FINANCES: England's hospitals are rapidly plunging into the red
At the end of the expansionary New Labour days, austerity arrived and the rapid growth of NHS spending slowed to a crawl. But hospitals’ books did not immediately indicate any great distress. For a time, small surpluses suggested they had learned to do more with less. But in 2013/14 the surpluses vanished, and a small average deficit crept in. By last year, this had ballooned to £2.5bn, and the real figure—once we strip out Whitehall’s bailouts, which will have to be repaid—is more like £3.5bn, or about 5 per cent of hospitals’ budget. The deficit is not concentrated in a few institutions: the vast majority are now running overdrafts. They have limited flexibility and little obligation to close wards or A&E doors. So the crisis plays out through drift—with the NHS spending as if it could print its own money, running up a tab the Treasury will not tolerate forever.
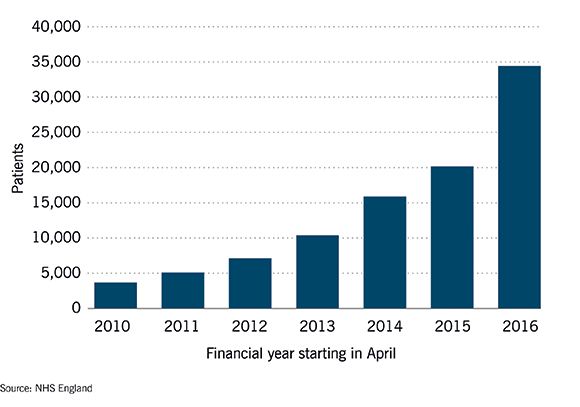
SERVICE PERFORMANCE: Patients are beginning to suffer Danger lights are flashing on all sorts of indicators of quality, from long delays in A&E to excessive waiting times for operations. But this chart looks at “trolley waits,” the number of patients stuck in the no-man’s land between the emergency department and the ward, waiting in corridors for between four and 12 hours. It is an interesting gauge of the whole system because it reflects not only the increased pressure of numbers coming through the front door, but also the blocking of beds at the other end. Inadequate care and medical services in the community prevent patients being discharged, which means fewer free beds, and more patients left on trolleys. This is a number that has been growing exponentially. The “trolley tally” is up 10-fold since 2010—and that is stripping out seasonal variation by looking at August alone.
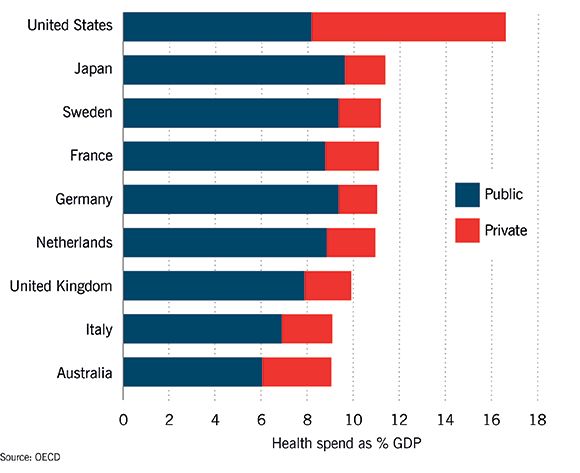
THE FUTURE: Look abroad and this doesn't look impossible to fix Healthcare is bound to cost more as society ages, especially when medicine keeps learning to do new and costly things. But that doesn’t mean it can’t be afforded. Since the inception of the NHS, demographics and technology have been pressures, and yet until 2010 it proved “affordable” to raise spending at an annual average of 4 per cent: faster than the economy grew. The long squeeze since 2010 is an aberration, which—under current plans—will shrink by a total of 0.9 per cent of GDP by 2020. The real constraint is willingness to pay, through tax or in other ways. Look abroad, and the UK does not seem a big spender—rather the reverse. Our publicly-funded spending is more than in, say, Australia, but is 1-2 per cent of GDP less than in Germany and many others. Gradually raising tax-funded spending to that tune would end the great squeeze. More private spending is the other option, which the United States pursues to a dramatic extent. But note how wasteful the American route is: they spend more than four times than we do privately, but still have to spend as much (in fact a touch more) than we do publicly.












